Phosphatidylethanol (PEth)
What is PEth?
Phosphatidylethanol (PEth) is a specific alcohol marker that can be detected in the blood. It is produced exclusively in the body when alcohol (ethanol) is consumed, as PEth is only formed through a reaction between ethanol and phospholipids in cell membranes.
PEth is considered a very specific marker for alcohol consumption. Unlike other alcohol markers, PEth is measured in the blood and can be detected for a longer period of time – up to several weeks – after the last alcohol consumption. Detectability depends on the amount consumed and the frequency of consumption.
These characteristics make it a valuable tool for the objective assessment of alcohol consumption. PEth tests are frequently used in traffic medicine, as part of abstinence testing, or in therapy monitoring. A positive PEth value reliably indicates relevant alcohol consumption.
The most reliable biomarker for long-term detection of alcohol
Why diagnosing alcohol consumption is important.
The diagnosis of alcohol consumption is of great importance from a medical, psychological, social, and legal perspective. A key reason for this is the far-reaching health consequences that chronic or excessive alcohol consumption can cause. Alcohol abuse is associated with numerous physical illnesses such as liver damage (e.g., fatty liver, hepatitis, cirrhosis), pancreatitis, cardiovascular disease, and an increased risk of various types of cancer. Mental well-being can also be severely impaired—for example, by depression, anxiety disorders, or personality changes.
Early and reliable diagnosis makes it possible to identify people at risk and initiate appropriate therapeutic measures. Particularly in the case of addiction disorders, accurate recording of consumption patterns is crucial for planning and implementing successful treatment.
Diagnostics also play a central role in traffic medicine, for example in assessing fitness to drive. Here, undetected or downplayed alcohol consumption can have serious consequences for public safety. Diagnostic procedures such as PEth, EtG, or CDT enable objective statements to be made about consumption, even if those affected do not disclose it themselves.
Determination of alcohol consumption is also highly relevant in social and professional contexts—for example, when assessing a person’s ability to work or evaluating family stressors. In certain occupational groups, alcohol consumption can be particularly risky under certain circumstances, which is why regular checks can be useful.
Ultimately, reliable diagnosis serves not to stigmatize, but to protect and help—both those affected and those around them. It enables individual prevention, targeted intervention, and long-term rehabilitation.
Direct and indirect biomarkers
Alcohol biomarkers are measurable substances in the body that provide information about alcohol consumption. They are used in diagnostics to objectively record alcohol consumption—whether in the medical, forensic, or traffic medicine fields. A distinction is made between direct and indirect alcohol biomarkers, which differ in their origin, significance, and detectability.
Direct alcohol biomarkers arise exclusively in connection with the consumption of ethanol. They are biochemical compounds that are only formed in the body when alcohol has actually been consumed. The best-known direct markers include phosphatidylethanol (PEth), ethyl glucuronide (EtG), and ethyl sulfate (EtS). These markers can be detected in blood, urine, or hair. Their great advantage is their high specificity: a positive test result means with a high degree of certainty that alcohol has been consumed. In addition, they provide information about the amount and frequency of consumption, depending on the substance and test method.
Indirect alcohol biomarkers, on the other hand, are biochemical changes in the body that can occur as a result of chronic or heavy alcohol consumption. They are not caused by the alcohol itself, but by its effect on the metabolism or organs. Typical indirect markers are gamma-glutamyltransferase (GGT), carbohydrate-deficient transferrin (CDT), MCV (mean corpuscular volume), or liver values such as ALT and AST. These values can also be influenced by other diseases or lifestyle factors and are therefore less specific. They are particularly suitable for detecting long-term alcohol abuse and for monitoring progress during withdrawal therapies.
In summary, direct markers provide concrete evidence of alcohol consumption, while indirect markers tend to indicate alcohol-related changes in the body. In practice, both groups of markers are often combined to obtain as comprehensive a picture as possible of consumption behavior.
| Marker | Matrix | Direct/ Indirect | Detection Period |
| PEth (Phosphatidylethanol) | Blood | Direct | up to 3 – 4 weeks |
| EtG (Ethylglucuronide) | Urine | Direct | up to 3 – 5 days |
| EtG (Ethylglucuronide) | Hair | Direct | up to 3 months |
| EtS (Ethylsulfate) | Urine | Direct | up to 3 days |
| FAEE (fatty acid ethyl ester) | Hair | Direct | up to 3 months |
| CDT (Carbohydrate-Deficient Transferrin) | Serum | Indirect | ca. 2–3 weeks (with chronic consumption) |
| GGT (Gamma-Glutamyltransferase) | Serum | Indirect | increases after weeks or months |
| MCV (mean corpuscular volume) | Blood | Indirect | increases after approx. 1–2 weeks, slowly returns to normal |
| AST (Aspartat-Aminotransferase) | Serum | Indirect | depending on consumption history |
| ALT (Alanin-Aminotransferase) | Serum | Indirect | depending on consumption history |
PEth in the body – Formation and Breakdown
The anabolism of phosphatidylethanol (PEth) is a special biochemical process, as PEth is not one of the regular components of phospholipid metabolism, but is formed exclusively under the influence of ethanol in the body. It is therefore an ethanol-induced synthesis, which makes PEth a direct alcohol marker.
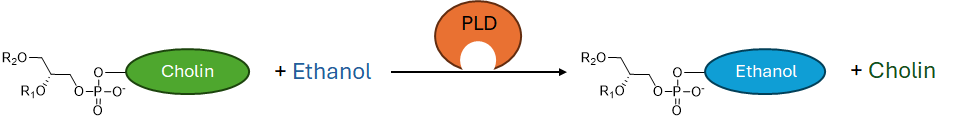
PEth is formed in the cell membrane by the enzyme phospholipase D (PLD). Under normal conditions, PLD catalyzes the hydrolysis of phosphatidylcholine (PC) to phosphatidic acid (PA) and choline. However, when ethanol is present in the body—for example, after alcohol consumption—the activity of this enzyme is affected: Instead of using water as a reaction partner, PLD now uses ethanol. This leads to the conversion of phosphatidylcholine into phosphatidylethanol (PEth) and choline. This process is specific to the presence of ethanol, making PEth a highly specific method for detecting alcohol consumption.
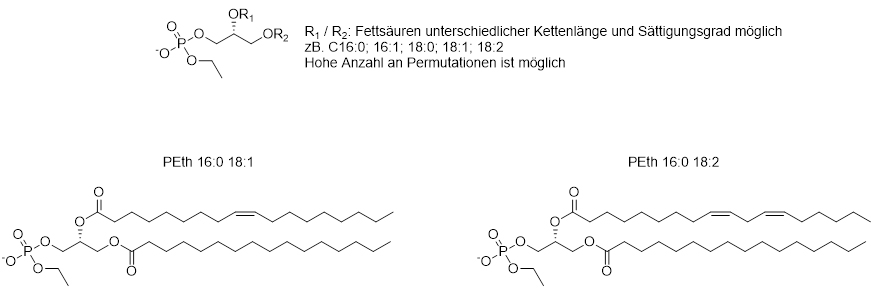
PEth accumulates in the cell membrane and remains relatively stable there. It is distributed predominantly in the membranes of erythrocytes (red blood cells), where it can be detected for days to weeks. The specific type of PEth molecule depends on the fatty acid residues of the starting material, which is why there are different PEth homologs (e.g., PEth 16:0/18:1). These are quantitatively determined in the laboratory using LC-MS/MS (liquid chromatography-tandem mass spectrometry).
The catabolism of phosphatidylethanol (PEth) is a relatively little-researched but nevertheless relevant aspect in understanding the metabolism of this direct alcohol marker. Unlike natural phospholipids, PEth is not part of regular cell metabolism, which is why its degradation processes (catabolism) do not follow the classic pathways of lipid utilization.
After synthesis, PEth primarily accumulates in cell membranes, especially those of erythrocytes. It is relatively stable there, as it is not regularly processed by enzymatic processes like other phospholipids. There is evidence that the degradation of PEth is predominantly non-enzymatic or non-specific enzymatic, e.g., by phospholipases or lysophospholipases, which are generally responsible for the turnover of membrane lipids. However, the exact mechanism has not been conclusively clarified. It is assumed that PEth remains in the cell membrane for a long time and is slowly broken down by cell turnover (e.g., through erythrocyte degradation in the spleen or liver) or by low enzymatic activity.
An important aspect of PEth catabolism is its long half-life. Depending on the study, this ranges from approximately 3 to 10 days, which means it can be detected for up to 3–4 weeks after the last alcohol consumption—depending on the amount consumed, the duration of consumption, and the individual’s metabolism. Unlike many other alcohol markers, PEth is therefore particularly well suited for retrospective analysis of alcohol consumption behavior, especially in cases of regular or heavy consumption.
In summary, it can be said that the catabolism of PEth is slow and nonspecific, primarily occurring through cellular renewal and membrane degradation processes, rather than through defined enzymatic metabolic pathways. This stability is one of the main reasons why PEth is such a reliable and sensitive marker in alcohol diagnostics.
Why PEth? – Advantages over other markers
Advantages of PEth over other direct alcohol markers (e.g., EtG, EtS):
- Longer detection time:
PEth can be detected in the blood for up to 3–4 weeks after chronic alcohol consumption—significantly longer than EtG/EtS in urine (only a few days). - High specificity for alcohol:
PEth is produced exclusively upon contact with ethanol—there are no false-positive results from non-alcoholic products or fermentation, as is the case with EtG. - No influence from liver function:
Unlike EtG/EtS, PEth is not dependent on liver metabolism and is therefore independent of liver disease or genetic differences. - Direct formation in the body:
PEth is only produced in living cells through a reaction with ethanol – it is therefore absolute proof of alcohol consumption. - Unaffected by short-term abstinence from drinking:
A short-term abstinence (1–2 days) is not sufficient to “mask” PEth – ideal for proof of abstinence.
Advantages of PEth over indirect alcohol markers (e.g., CDT, GGT, MCV):
- Significantly higher sensitivity and specificity:
PEth also reliably indicates moderate consumption, whereas indirect markers usually only react in cases of chronic alcohol abuse. - Rapid increase after consumption:
PEth levels rise within hours to days after drinking—indirect markers usually take weeks to change. - No influence from other diseases:
Markers such as GGT or MCV can also be altered by liver disease, medication, or other influences—PEth is alcohol-specific. - No daily or laboratory value fluctuations:
PEth is less susceptible to fluctuations that can occur in liver enzymes or blood count components, for example. - Clear results:
While indirect markers often require interpretation, PEth provides direct and quantitative evidence of alcohol consumption.
PEth is increasingly being used in diagnostics—both in clinical practice and in forensic or occupational medicine contexts.
Areas of application
PEth is used in a variety of medical and legal contexts:
Addiction medicine: Progress monitoring and relapse monitoring
Traffic medicine: Assessment of fitness to drive (MPU, medical-psychological examination))
Organ transplantation: Abstinence test before or after transplantation
Forensics: Court proceedings or probation checks
Prenatal diagnostics: Detection of alcohol consumption during pregnancy
Science/research: Collection of objective alcohol consumption data in studies
FAQ – Frequently asked questions about PEth
How long is PEth detectable?
Depending on consumption habits, up to 3–4 weeks after the last consumption of alcohol.
What distinguishes PEth from other markers such as EtG or CDT?
PEth combines the advantages of a direct biomarker such as ETG with high specificity and a longer detection time such as CDT.
Can PEth become positive through non-alcoholic products (e.g., non-alcoholic beer)?
No. It is only formed through significant ethanol contact.
How can PEth diagnostics be implemented?
For help and information on PEth diagnostics, send us a message via the website or email us at info@archimedline.com.
References
- Helander A, Hansson T. National harmonization of the use of the alcohol biomarker PEth. Alcohol Alcohol. 2013.
- Varga A, Alling C. Formation of phosphatidylethanol in human red blood cells incubated with ethanol. Alcohol Clin Exp Res. 1990
- Helander A, Zheng Y. Molecular and clinical aspects of phosphatidylethanol as a biomarker of ethanol intake. Clin Chim Acta. 2009.
- Viel G, Boscolo-Berto R, Cecchetto G, et al. Performance of phosphatidylethanol (PEth) as a biomarker for chronic alcohol abuse. Clin Chim Acta. 2012.
- Schröck A, Wurst FM. Use of PEth in clinical and forensic settings. Int J Legal Med. 2020.
- Aradottir S, Seidl S, Wurst FM. Phosphatidylethanol in blood as a marker of ethanol consumption. Alcohol Clin Exp Res. 2006.
- Deutsche Gesellschaft für Suchtforschung und Suchttherapie (DG-Sucht): Leitlinien zur Diagnostik und Therapie von Alkoholabhängigkeit. https://www.awmf.org/leitlinien
- Verkehrsmedizinische Begutachtung (Krause, L. et al.) – 4. Auflage
- Behrendt, S. et al. Markers of chronic alcohol consumption in blood: Ethanol, PEth, CDT, GGT, and MCV. Forensic Science International. 2010.
- Wurst, F.M., et al. Alcohol biomarkers in clinical and forensic settings. Trends in Molecular Medicine. 2015.
- Hoiseth, G., et al. Phosphatidylethanol (PEth) in blood as a marker of alcohol use: A review of PEth in medical and forensic settings. Alcoholism: Clinical and Experimental Research. 2008
- Substance Abuse and Mental Health Services Administration (SAMHSA). The Role of Biomarkers in the Treatment of Alcohol Use Disorders. Report, U.S. Department of Health and Human Services. https://www.samhsa.gov
- Hartmann S. et al. BIOMARKER: Phosphatidylethanol as a sensitive and specific biomarker—comparison with gamma-glutamyl transpeptidase, mean corpuscular volume and carbohydrate-deficient transferrin. Addiction Biology 2007
- Isaksson A. et al. Phosphatidylethanol in blood (B-PEth): A marker for alcohol use and abuse. Drug Test Analysis. 2011
- Helander A, et al. The alcohol biomarker phosphatidylethanol (PEth) – recommendations for use and interpretation of test results. Lakartidningen. 2023
- Årving, A. et al. Comparison of the Diagnostic Value of Phosphatidylethanol and Carbohydrate-Deficient Transferrin as Biomarkers of Alcohol Consumption. Alcohol Clin Exp Res. 2021
- Perilli M. et al. Phosphatidylethanol (PEth) in Blood as a Marker of Unhealthy Alcohol Use: A Systematic Review with Novel Molecular Insights. Int J Mol Sci. 2023
Send us a message.
 GmbH
GmbH